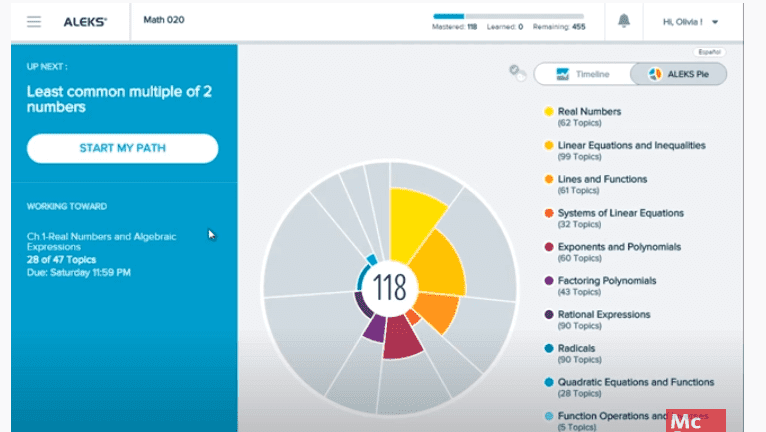
ALEKS Answers Key 2023: Access for Free and Ace Your ALEKS Exam
Looking for ALEKS answers key to ace your ALEKS exam? Find out how to access ALEKS homework help and answers for free in 2023, and boost your math skills and score today!
Read MoreIt takes some brainstorming, research, and planning to identify a clinical problem that can be translated into PICOT questions. The word PICOT is derived from the elements of a clinical research question – patient, intervention, comparison, outcome, and (sometimes) time.
Registered nurses begin their research questions using an evidence-based practice framework developed from a well-constructed PICOT question. The process begins with a case scenario, and the question is phrased to elicit an answer. The question identifies the patient or population of study, the treatment to be used, and the anticipated outcome comparison.
Formulating these questions places the researchers in a better position to search the literature for evidence supporting their original PICO question. This article focuses on helping clinicians with a compelling desire to pursue research within their profession and the entire health system.
Clinicians' involvement in formulating research questions, interpreting results, and moving research findings into practice. This shared effort between clinicians and researchers increases the likelihood that research initiatives will be relevant to practice and prompts clinicians to base their decisions on the best available scientific evidence.
Lack of clinician representation in research has the probable effect of limiting growth and new developments for the profession and complicates the transfer of study findings into practical settings
Cooperation can help bridge the growing communication gap between clinicians and academics in chiropractic. Clinicians have important practice-related questions to ask, but many may lack the ability to map out their research strategy, specifically in communicating their questions in the manner required to develop a research protocol.
Identifying a clinical problem that can be translated into a PICOT question takes some brainstorming, research, and planning. The following recommendations can help in triggering ideas for your PICOT question:
· Patient cases you have encountered
· Clinical scenarios you have observed
· Quality improvement data
· Other internal data specific to your organization
· Conduct a search of the research literature to identify problems or practice recommendations
· Identify interventions that have been proven effective by previous studies
· Clinical practice guidelines recommendations
PICOT question serves as the foundation of your literature search strategy for your research project literature review by utilizing the key terminology from your PICOT components as database search terms. Only after a thorough literature synthesis and investigation into these answers should a research question be formulated – in some instances, a systematic review methodology may align best with the PICOT question format for your research question. Turning an idea into a good research question requires it to be feasible, ethical, and relevant. In addition, it is of interest to many in the clinical area to drive team momentum for the project and dissemination of the results.
(P) – Population refers to the patient population you wish to recruit for your study that is most likely to respond to your intervention or you are likely to see in actual practice. It would be best if you considered the population age , gender, ethnicity, and individuals with a certain disorder
(I) – Intervention refers to the treatment that will be provided to subjects enrolled in your study. Monitor the indicators of exposure to a disease, risk behavior, prognostic factor
(C) – Comparison identifies the main alternative being considered. Many study designs refer to this as the control group. ((e.g., placebo, standard therapy, no treatment, no disease or absence of risk factor. If an existing treatment is considered the 'gold standard,' this should be the comparison group.
(O) – Outcome represents what you hope to accomplish to examine the effectiveness of your intervention. The desired outcome can be the risk of disease, the accuracy of a diagnostic test, the rate of occurrence of adverse outcome
(T) – Time describes the perioperative and recovery time frame for the intervention to achieve an outcome or how long participants are observed.
A clinical question that is composed using the PICOT framework will help you to focus your search and help you to develop your research skills which are essential in finding the best available evidence. Importantly, Not every question will have an intervention (as in a meaning question or time (when it is implied in another part of the question) component.
· For instance, obese adoptive parents have an increased risk for obesity compared to kids without obese parents from ages five to 18.
· How do pregnant women (P) newly diagnosed with diabetes (I) perceive reporting their blood sugar levels (O) to their healthcare providers during their pregnancy and six weeks postpartum?
· Do nurses doing a five minute scrub (P) what are the differences in the presence and types of microbes (O) found on natural polished nails and nail beds (I) and artificial nails (C) at the time of surgery (T)?
· In adult patients with total hip replacements ( Population), how effective is pain medication ( I intervention) compared to aerobic stretching ( Comparison) in controlling post-operative pain ( O outcome) during the perioperative and recovery time ( Time)
· Is a PKU test (I) done on two-week-old infants (P) more accurate in diagnosis inborn errors in metabolism (O) compared with PKU tests done at 24 hours of age?
· For childern under the age of 6, does the use of antimalarial reduce the future risk of malaria compared with personal protective measures.
· In prognosis of blood pressure patients for six months. During this period telelmonitoring blood pressure, such as improved blood pressure control should be recorded. This will help control post-operative pain by taking pain medication to avoid future risks such as post-operative infection.
· Does telelmonitoring blood pressure (I) in urban African Americans with hypertension (P) improve blood pressure control within the six months of initiation of the medication (T)?
· What is the duration of recovery (O) for patients with total hip replacement who developed a post-operative infection (I) as opposed to those who did not (C) within the first six weeks of recovery (T)?
· After the PICOT question is constructed and researched, the information garnered is used to determine which type of study is most appropriate. Study types include meta-analysis, systematic review, randomized controlled trial, cohort study, case-control study, and case report.
To develop a strong research question framed in the PICOT format, it is important to understand the clinical area of investigation and the current literature. It is necessary to review the type and quality of research already performed in the area of interest to guide the development of a question. When initially synthesizing the literature, some key entry questions to examine include:
· What are the important research questions in the field?
· What has been found?
· What areas need further exploration?
· Would the proposed study fill a gap and better an understanding
The PICOT format represents a factorial RCT methodology formulated by the existing literature. A well-conducted RCT research method can answer many questions on treatment efficacy. However, some of this methodology's major disadvantages are the cost and time and are generally challenging to conduct. Additionally, not all research questions clinicians wish answered are feasible using this research methodology.
The clinical research question being asked ideally determines the best research design for a study. For example, a prospective or retrospective cohort design may be an easier methodology to administer compared to an RCT. Still, study results can be affected by confounding due to the comparison of non-randomized groups.
This methodology is used for associations between respondent features and results of interest. This methodology is faster and less expensive than an RCT since it considers one time-point of individuals in various aspects of the variables of interest. However, this design can also be prone to recall problems by respondents who self-report information if investigators ask about events in the past.
This is the most appropriate methodology for identifying associations between patient characteristics and outcomes that take a long time to occur or are very rare.
Generating new knowledge in large existing healthcare gaps provides the opportunity to help large volumes of patients who previously may have had poorer clinical outcomes. Ethical considerations must be accounted for in related study designs to ensure the study does not harm subjects. A well-thought-out focused research question leads directly into hypotheses, the predictions about the nature and direction of the relationship between the variables under study. Finally, reflection is required on how well the study design will apply to the real world.
Clinicians interested in research pursuits related to patient care should consider using a literature search and the PICOT format when engaging clinical researchers. A clinical question that is composed using the PICO or PICOT format will help you to focus your search and help to develop your research skills which are essential in finding the best available evidence. This approach will provide clinicians and researchers an initial basis for mutual understanding, communication, and direction to help answer clinical study questions of the most relevance
Get affordable and top-notch help for your essays and homework services from our expert tutors. Ace your homework, boost your grades, and shine in online classes—all with just a click away!



Fast, secure, and handled by vetted experts.
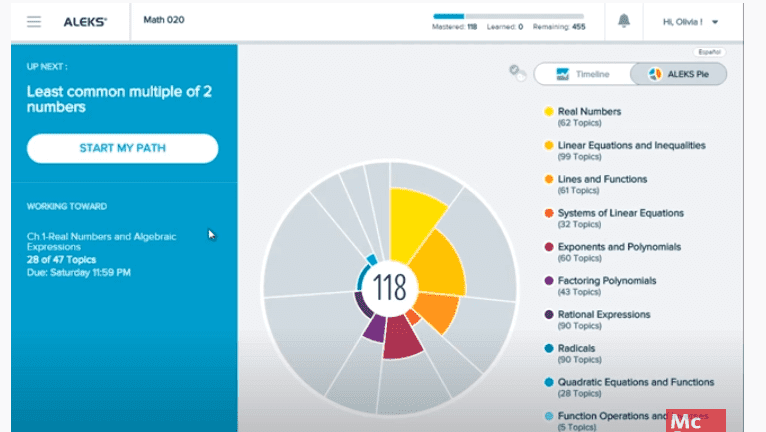
Looking for ALEKS answers key to ace your ALEKS exam? Find out how to access ALEKS homework help and answers for free in 2023, and boost your math skills and score today!
Read More.jpg)
Discover the ultimate guide to studying effectively for the SAT with expert tips, tricks, and techniques from AceMyHomework. Boost your score and secure your dream college spot!
Read More
As a college student, staying on top of your studies can be a challenge. These 10 innovative study techniques can help you study smarter, not harder, and improve your academic performance. Get the homework help you need!
Read More